ReCredentialing and Contracting



2x Faster Re-Credentialing – Stay Active & Paid Without Delays
Stay Compliant, and Focus on Patient Care
Re-credentialing is a mandatory, recurring process required by insurance networks to verify that healthcare providers continue to meet credentialing standards. If not completed on time or accurately, your participation status can be jeopardized—leading to claim denials or termination from payer networks.
At States Credentialing, we make re-credentialing easy. Our team monitors deadlines, updates your documentation, and ensures everything is submitted accurately and on time. We also handle payer contract renewals, renegotiations, and credentialing updates—so your practice remains compliant and profitable.
What is Re-Credentialing?
Re-credentialing is the periodic re-verification of a provider’s qualifications by insurance payers, typically required every 2-3 years. It ensures ongoing compliance with the payer’s standards and is crucial for uninterrupted reimbursements
Our team manages this process on your behalf, ensuring applications are submitted correctly and on time to keep your credentials active and your revenue flowing.
Why Choose
States Credentialing for Re-Credentialing & Contracting?
Credentialing isn’t just a one-time task—it’s an ongoing responsibility that demands accuracy, compliance, and consistency.
At States Credentialing, we take the stress out of maintaining your credentials by offering complete re-credentialing and contract management services. Our team tracks deadlines, handles communications with payers, updates your documentation, and ensures you remain compliant—so you can avoid costly delays or network terminations.
Fast & Hassle-Free Re-Credentialing
We manage the entire re-credentialing cycle from start to finish—tracking deadlines, collecting updated credentials, and ensuring all submissions are made on time to prevent lapses in network participation.
Compliance & Accuracy
Our experts ensure every application meets payer-specific guidelines to minimize errors, rejections, or compliance issues.
Complete Re-Credentialing Support
From CAQH updates to payer communication, we handle it all.
Contract Negotiation & Renewal
We review, update, and negotiate contracts to help you get paid more—on time.
Nationwide Coverage
We serve individual providers and group practices across the entire U.S.
Dedicated Credentialing Specialists
Our credentialing specialists work closely with you throughout the re-credentialing and contracting process.
Get Re-Credentialed On Time – Without the Headache
Let our credentialing team manage the process, keep your contracts current, and help you avoid compliance risks.
Seamless Re-Credentialing with Leading Insurance Networks
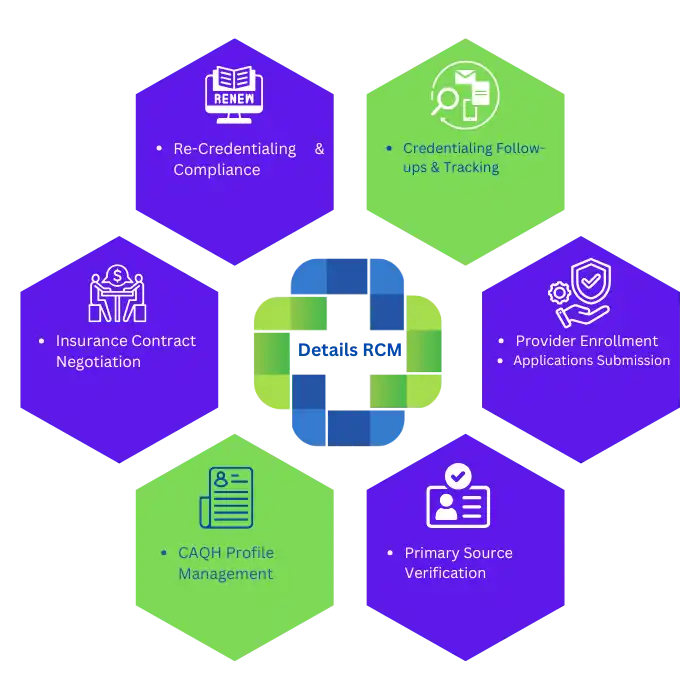
States Credentialing offers comprehensive re-credentialing and contract management services across all major insurance companies. We handle every step application resubmission, primary source verification, CAQH profile updates, contract review, and payer communication so your participation stays uninterrupted and profitable.






How Our Credentialing Process Works
Lorem Ipsum is simply dummy text of the printing and typesetting industry. Lorem Ipsum has been the industry’s standard dummy text ever since.
1
Identify Provider & Specialty
We begin by reviewing your provider type, specialty, and network history to tailor a re-credentialing plan.
2
Document Review & Updates
Our team collects and updates all necessary documents, including licenses, DEA, malpractice insurance, and CAQH profiles.
3
Re-Credentialing Submission
We handle all payer applications, coordinate verifications, and respond to any requests or corrections.
4
Contract Management
We ensure your contracts are renewed, updated, or renegotiated, and we provide complete visibility into the process with regular updates.
Other credentialing Services
We understand that every provider’s needs are different. Our goal is to simplify credentialing for you and keep your practice running smoothly.

Provider Credentialing
we’ll make sure your enrollment process is stress-free and professionally managed from beginning to end.

CAQH Profile Setup & Maintenance
Let us take the hassle out of managing your profile so you stay accessible to insurers at all times.

Insurance Credentialing
We work directly with all major insurers to get your application submitted, followed up, and approved as quickly as possible.

Medicare & Medicaid Enrollment
Our experts guide you through the enrollment process step by step, ensuring your documentation meets all federal and state guidelines.

Recredentialing & Contracting
We monitor your renewal dates, prepare required documents, and submit everything on time—ensuring your services remain uninterrupted and fully compliant with payer requirements.

Hospital Privileging Services
Our team ensures your hospital privileging is approved efficiently, so you can continue practicing with confidence.
