Prodvider Credentialing Company in USA
Your Trusted Partner for Easy Healthcare Credentialing in New York
Sates Credentialing is a leading provider credentialing company in New York, offering efficient, accurate, and compliant solutions that simplify the credentialing process for healthcare professionals, ensuring faster approvals and peace of mind.
1
Provider
Information Collection
- NPI & DEA numbers
- State medical licenses
- Educational qualifications
- Board certifications
- Work history
- Malpractice insurance
- Hospital privileges
- Disclosure of legal issues
2
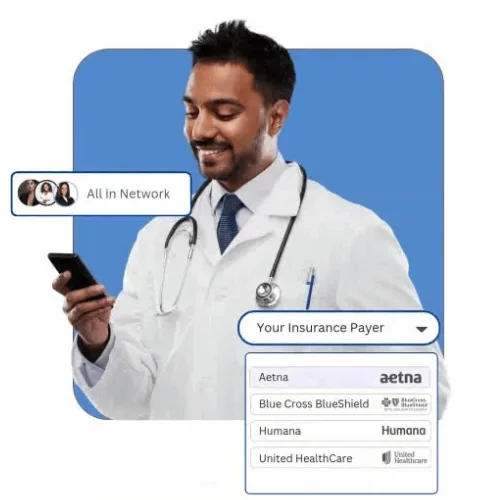
Insurance
Panel Enrollment
- Payer research & requirements
- Network participation requests
- Network participation requests
- Application form submission
- Follow-up with insurance reps
- Documentation verification
- Reimbursement agreements
- Approval notification tracking
3
Ongoing
Recredentialing Maintenance
- License renewal tracking
- CAQH re-attestation
- Insurance re-credentialing
- Monitoring expirations
- Compliance with payer rules
- Update demographic info
- Timely document submissions
- Credentialing audits support
Why Choose States Credentialing Inc. — Trusted by Practices Nationwide
With years of experience in managing credentialing for healthcare providers, we have refined our process to deliver exceptional results through:

Tailored Credentialing Solutions
We customize our credentialing services to meet the unique needs of each healthcare provider, ensuring efficiency and timely enrollments.

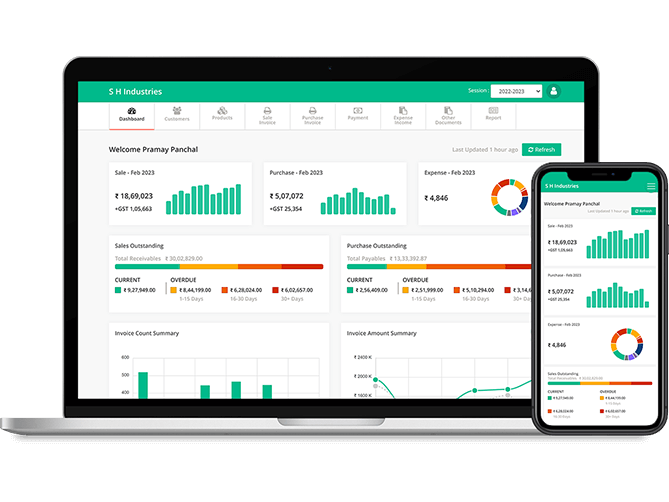
Technology-Driven Credentialing
Leveraging AI tools and automated workflows, we streamline applications, track progress in real-time, and reduce errors—helping providers get credentialed faster and more efficiently.
Proactive Denial Prevention & Follow-Up
Our team monitors all credentialing applications, addresses errors proactively, and follows up with payers to prevent denials and delays, ensuring uninterrupted participation and revenue.

Compliance & Regulatory Expertise
We ensure all credentialing applications adhere to HIPAA, CMS, and payer-specific rules, minimizing compliance risk while maximizing timely approvals and reimbursements.
Top-Notch
Credentialing Solutions
to Support Your Practice Growth
Streamline your provider enrollment, payer contracting, and credentialing renewals with expert support. States Credentialing ensures accuracy, compliance, and faster approvals so your practice can focus on patient care.

Mental Health
Streamlined billing solutions for psychiatrists, therapists, and mental health clinics.

Obstetrics & Gynecology
Hassle-free billing services for OB/GYN physicians and women’s health.

Dermatology
Accurate claim processing and coding solutions for dermatology practices.
Interventional Pain
Optimized reimbursements for pain specialists and pain management clinics.

Orthopedics
Complete RCM for orthopedic surgeons and musculoskeletal providers.

Gastroenterology
Specialized billing solutions for GI specialists and endoscopy centers.

Ophthalmology
Efficient billing services for eye care professionals and vision centers.
End-to-End
Insurance Credentialing, Contracting, and Recredentialing Support
At States Credentialing LLC, we provide customized medical credentialing services tailored to meet the needs of healthcare providers nationwide. Our mission is to simplify the provider enrollment process, reduce administrative delays, and ensure smooth payer participation with accuracy and compliance. From insurance credentialing and CAQH setup to contracting, recredentialing, and hospital privileging, our end-to-end credentialing solutions help your practice get enrolled faster, stay compliant, and maintain active network status effortlessly.

Commercial
Insurance Credentialing
From patient registration to final payment, we provide complete guidance and support at every stage of your revenue cycle process.

ReCredentialing
Contracting Solutions
We assist healthcare providers in completing credentialing with all insurance networks, ensuring they can accept every patient without interruptions or delays.

CAQH Profile
Setup and Maintenance
Our experts perform detailed RCM audits to uncover revenue leaks, compliance risks, and inefficiencies that impact overall collections and cash flow.

Provider
Credentialing Services
We also help practices enhance workflow efficiency, patient retention, and develop strategic growth plans for long-term success and stability.
Nationwide Credentialing Solutions
We provide fast, reliable credentialing services for providers across the U.S., helping you stay compliant, contracted, and ready to serve patients. Our team supports healthcare professionals in New York, California, Texas, Florida, Georgia, Illinois, Pennsylvania, North Carolina, New Jersey, and Virginia, ensuring smooth enrollment, contracting, and ongoing recredentialing with all major payers.
- Availibility
- Responsiveness
- Reliable
- Support
States Credentialing delivers end-to-end provider credentialing services to simplify insurance enrollment for healthcare professionals. Our experts manage the full process — from application submission and CAQH maintenance to primary source verification and contract negotiation — ensuring faster network participation, regulatory compliance, and seamless payer integration for improved revenue cycle efficiency.
Simplify your billing process and maximize revenue with our expert RCM solutions. From credentialing to claims management, we handle every step to ensure faster reimbursements and fewer denials. Partner with us for a seamless, efficient revenue cycle—so you can focus on patient care.
1

Accurate Coding
Avoid costly mistakes with accurate medical coding that adheres to payer regulations, minimizing claim denials and boosting reimbursement rates.
2

Claim Scrubbing
Ensure every submission is error-free with automated claim validation, detecting and correcting issues before reaching payers.
3

Denial Management
Recover missed income through denial tracking, analysis, and strategic appeals for quicker, complete payments.
4

Eligibility Checks
Reduce rejections by verifying insurance eligibility upfront, preventing delays and unexpected payment issues.
Why Providers Trust
with States Credentialing
With years of experience in managing credentialing for healthcare providers, we have refined our process to deliver exceptional results through:

State-Specific Payer Expertise
We understand each state’s payer rules, ensuring faster approvals and fewer compliance issues.

Error-Free Application Processing
Every application is reviewed and verified to eliminate mistakes that commonly cause delays.
Dedicated Credentialing Specialist
You get a single point of contact who manages your entire credentialing journey from start to finish.

Faster Enrollment Turnaround
Our optimized workflows and payer relationships help you get credentialed and contracted more quickly.
Ready to Grow?
Get Credentialed Without the Hassle
Expand your payer network, increase patient volume, and avoid preventable denials—starting today.
Software We Use
Our team has expertise of major EHR software used in medical billing industry


























Every Provider We Serve
Becomes a Happy Story
We’re proud to support healthcare providers across the country with fast, reliable, and compliant credentialing services. Here’s what some of them told about us.





